Click on any question to see the answer:
1. When do I "need" a joint replacement?
2. What are the effects of genetics, wear and tear, and/or arthritis on my joints and what goes wrong when you have osteoarthritis?
3. How do I choose my joint replacement surgeon?
4. Should I have both knees replaced at once -- and what about having both hips replaced at once?
5. How do I prepare my home for safety and comfort after joint replacement?
6. What are my options for anesthesia in joint replacement?
7. What is the hospital stay like after total hip replacement or total knee replacement?
8. What physical therapy is needed for successful recovery from joint replacement and what is recovery like after joint replacement?”
9. What can go wrong with my hip replacement or knee replacement?
10. What will my life be like after hip replacement or knee replacement?

1. When do I "need" a joint replacement?
Covered in Chapter 1 - When Do You Know You "Need" a Joint Replacement?
As you age your joints wear out and arthritis can set in. Also, there are other types of arthritis which aren't related to age -- or maybe you have an old injury -- or previous joint surgery, that's finally come to a point where it has become debilitating for you.
- Dr. Hugate reviews what his patients tell him everyday and explains that there is a judgment call on the part of his patients as to how long they can continue to deal with the pain and issues that a worn out joint creates in their life.
- Mr Holland explains what he was going through in terms of not being able to get into his pickup using his right leg (the 'bad knee') and how hard it was after going for a bicycle ride (one of his favorite exercises).
- Dr. Francine Campone talks about the debilitating effects of deteriorating hip joints on her relationships and losing the ability to dance, one her favorite things in life.
2. What are the effects of genetics, wear and tear, and/or arthritis on my joints and what goes wrong when you have osteoarthritis?
About Chapter 2 - Nuts and Bolts of the Hip & Knee
A few things can happen that cause pain in joints. The bottom line is that the hip and knee joints are like well-oiled machines, but because they are so precise, they are also susceptible to problems if there are small changes (or even moderate deterioration). A fine Swiss watch would not tolerate a speck of loose dirt or a slightly bent gear and neither will your joints in the long term.
- A fracture (broken bone) that involves the joint can damage the articular cartilage and create arthritis because the joint surfaces will no longer align perfectly.
- You can certainly damage the cartilage of the joint without breaking the bone as well. If there is damage to a ligament whose job is important to stabilizing the joint, or if you dislocate a joint in an accident, it can become loose and this will cause arthritis because the bones will shift excessively and create wear and/or shearing of the cartilage.
- The effects of age, genetics, weight, and lifestyle can simply wear the cartilage to the point that it’s no longer effective.
- Hip and knee joints can sometimes be misshapen from birth in such a way that the cartilage wears more quickly over the average lifespan as well.
- These are just a few of the possibilities concerning what might be going on in your joints as you age.

3. How do I choose my joint replacement surgeon?
About Chapter 3 - How to Go About Selecting a Surgeon, Do's and Don'ts
Dr. Hugate devoted an entire chapter to explaining how to go about finding your surgeon and tells you the 'best practices' for this critical decision.
Many regions and principalities have Orthopedic Surgery Centers and their surgeons will be excellent.
- Most states have a state department of regulatory agencies--check them online.
- Assess whether the new surgeon (whom you've just met) is open to 2nd opinions.
- Seek Referrals -- we tell you how.
- Do your own research -- we tell you where.
- Examine their credentials -- we tell you why.
- Ask Questions -- we suggest the best ones to ask.

4. Should I have both knees replaced at once -- and what about having both hips replaced at once?
About Chapter 5 - Two Knees or One?
There are many factors to consider. This decision should be made jointly between you, your PCP, your surgeon (and should also include any specialists whose care you are under) and some consideration about the need and cost of extended care afterward.
- Point-by-point, Dr. Hugate compares having one knee replacement versus two and how having one knee replaced can save the other.
- There is less anesthesia when it's two knees versus one, but there can be more bleeding -- and obviously, more time in the operating room.
- Time away from home and the need for staying in an extended care facility after having both knees replaced is an important consideration.
- Is the amount of co-pay associated with having 2 procedures at once a factor you should consider?
- Are you in good enough health to withstand the recovery and stress of two knee replacements?
- Do you have any condition that would be a factor?
- Lastly, Dr. Hugate explains why he does not support having two hips done at once.
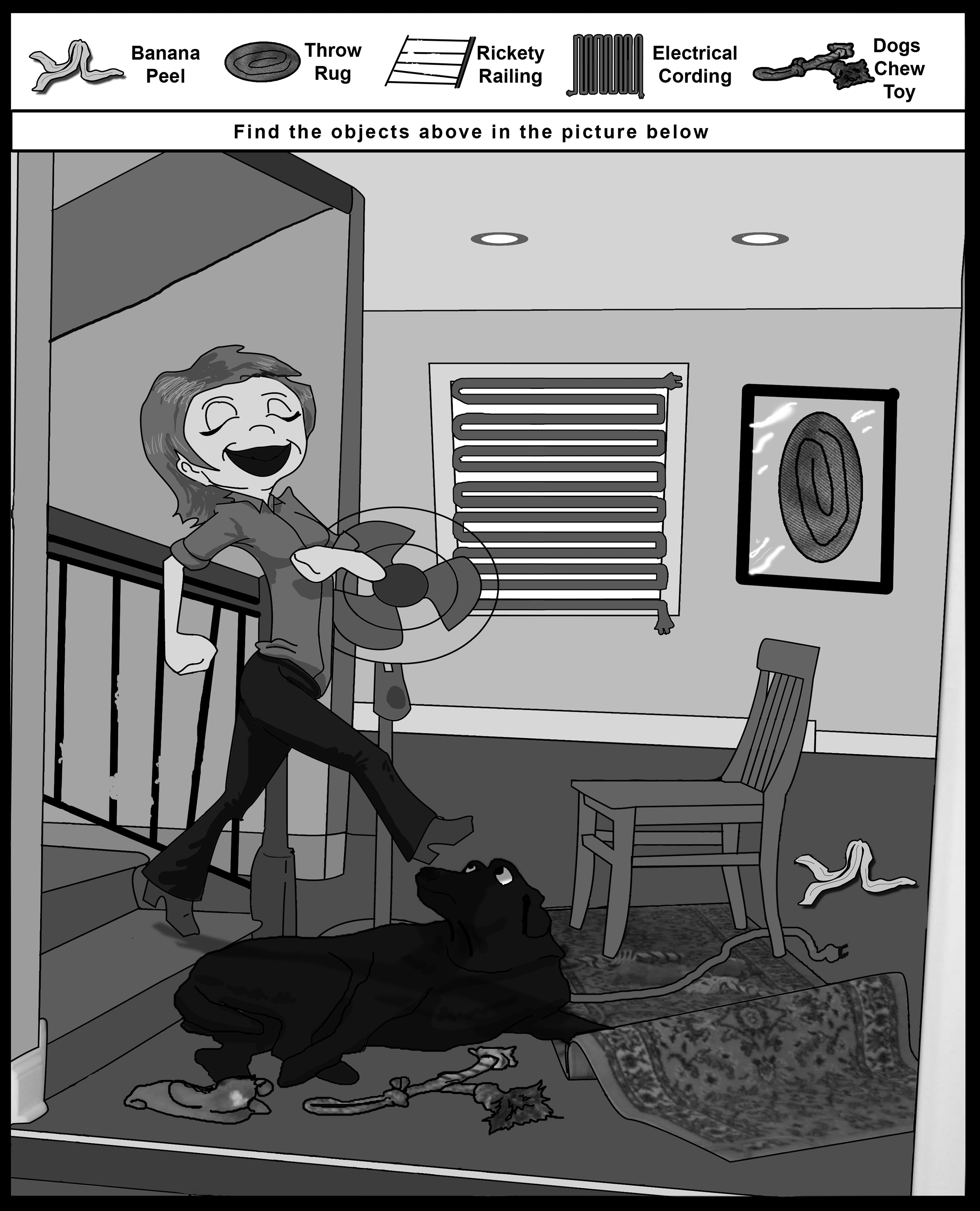
5. How do I prepare my home for safety and comfort after joint replacement?
About Chapter 8 - Preparing Your Home
Clikc to see the "2010 ADA Standards for Accessible Design"
Most people never really assess their home in the manner most businesses must do in becoming compliant with the Americans with Disabilities Act (ADA), and yet, there is a great deal you can do to get your home prepared before going in for your procedure and the ADA is a great starting place.
- Are there any stairs?
- If there are stairs, do they have secure handrails?
- Are the carpet runners?
- Are there throw rugs at the top or bottom?
- All tripping hazards must be removed, a trip-and-fall incident could seriously affect your recovery.
- Are your bathrooms safe and secure with strong grab bars instead of weak, spindly towel racks?
- Are there grab bars where you step in and out of your tub? Your shower?
- Is the house cluttered with pets toys and bowls?
- Are there small grand children who need to be trained about the issues associated with your recovery?
- Robert explains why these are issues after THR (Total Hip Replacement), or TKR (Total Knee Replacement) and what you can and should do about them.

6. What are my options for anesthesia in joint replacement?
About Chapter 9 - Anesthesia Options in Joint Replacement Surgery
You should consider an extended discussion between you and your surgeon to discuss your options and preferences -- and to discuss his or her preferences as your surgeon as well -- and remember: it can include your anesthesiologist.
However, waiting until you're inside the pre-operative prep-room and ready to operated on is the wrong time to start thinking about your options -- provided you even know what they are -- its too late! In this chapter Dr. Giancarlo Checa covers these options in great detail and easily understandable language.
- You can have 'general anesthesia' and be asleep when the surgery is done.
- You can remain awake--while heavily sedated--and not be 'put out' while the procedure takes place--which would include what is known as a 'spinal block'.
- You can also have a local 'nerve block' for when you wake up from surgery and this very dramatically reduces post-operative pain.

7. What is the hospital stay like after total hip replacement or total knee replacement?
Covered in Chapter 13 - The Hospital Stay
Robert takes you on his journey through the hospital stay mid-2009 (when he had right knee joint replaced); and Dr. Hugate explains what was going on from the surgeon's point-of-view. Written in first person, this up close and personal story is both captivating and enlightening because -- for the first time we know of -- you get to feel what the patient feels day-by-day, hour-by-hour, and you get to know his team of caregivers as they watch over him and get him right back on his feet.
Robert tells the story of what it was like waking up after his total knee replacement and you're right there with him as he regains consciousness.
- He describes how Dr. Hugate guided him on his choices for pain management after the second TKR and how it made the experience so much less painful (by using a local nerve block in his right leg with a small pump to deliver the pain reliever through a tiny catheter in his thigh).
- You'll get to know the in-hospital physical therapist, how Robert felt, and why the therapist had Robert on his feet the very next day after surgery.
- You'll meet Robert's occupational therapist and how both she and his physical therapist evaluated him (as a team) to determine if Dr. Hugate would consider him 'ready' to go home -- and how this was all based on Robert's ability to handle his ADLs ( Activities of Daily Living).
8. What physical therapy is needed for successful recovery from joint replacement and what is recovery like after joint replacement?”
Covered in Chapter 14 - Physical Therapy, for Hip and Knee Surgery
Physical therapy (PT) and occupational therapy (OT) are both absolutely critical to having a good outcome from your hip replacement or knee replacement. Therapy begins the day you wake up in the hospital and continues for at least 5-6 weeks -- sometimes more if needed. During this critical period after surgery, you must be very complaint with your PT's and OT's instruction -- neither doing too much nor too little. In this case, your therapist truly knows best!
Just like anything in life, the more you put into it, the more you'll get out of it, find out why in much greater detail and answer this question: Is there any point in going through a hip replacement or knee replacement if you're not going to put in the effort afterward to have the best possible results?
- We'll explain what a Continuous Passive Motion Machine (CPM) is, how it's used, and how it works. However, in the first two weeks after surgery it will be an important component of your recovery.
- When recovering from hip replacement, there are prohibited motions concerning bending over.
- Your position when sleeping after hip replacement could cause your new hip implant to be dislocated, i.e. you must not cross your legs. Find out why!
- How your hold your feet after hip replacement can prevent a dislocation of the new hip implant too -- and there is so much more to know.
9. What can go wrong with my hip replacement or knee replacement?
Covered in Chapter 15 - What Can Go Wrong
While there are a lot of things that can go wrong, your physicians, nurses and therapists will be watching very carefully over you at all times. Dr. Hugate fields questions about these risks everyday in his clinic and manages these risks for his patients every day.
- For the first time we know of, a physician has truly taken the time to explain these most common risks and Dr. Hugate also takes the time to instruct you, the reader, how these are managed.
- Yes, this is the bare bones truth -- but the authors and collaborators want you to know that this handbook is not a commercial for hip replacement or knee replacement -- but is written to empower the patient in making the best decisions possible for themselves and their loved ones.
- Infection can be a problem, but only occurs in the tiniest fraction of the hip replacement and knee replacement surgeries--your surgeon and his team will be taking every possible precaution.
- Your dental health factors into your upcoming surgery because teeth and gums are a gateway for potential problems?
- You might need a blood transfusion and you and your surgeon will discuss the possibilities and various options concerning your needs and preferences.

10. What will my life be like after hip replacement or knee replacement?
Covered in Chapter - 16 Life After Joint Replacement
Dr. Hugate, "Even though you’re done with your joint replacement, there are some things you need to be aware of going forward. Not too much to know—just a few minor issues. This chapter of the handbook will address the ongoing maintenance of your joint replacement after you’ve fully recovered from THR or TKR and also identify a few 'land mines' for you to dodge. Keeping a copy of this handbook and looking back on this chapter every so often is not a bad idea. Having a knee or hip replacement is like buying a new car in many ways."
- As we've said before, your dental health is a factor before surgery, but it continues to be a factor forever after. Get yourself a good water-jet dental irrigator and use a good, anti-bacterial mouthwash in it and brush your teeth very well everyday.
- Follow your surgeon's instructions for visits with your dentist, but keep in mind that Dr. Hugate recommends his patients to pre-medicate with antibiotics before even so much as a teeth cleaning. This is because bacteria can get into your bloodstream through the gums when the dentist or hygienist is working on your mouth.
- The same argument as above holds true for any surgical procedure [you have done] which breaks the skin--be sure to discuss this with your surgeon and let your other medical caregivers know about your joint replacement before you have anything done.
- See your surgeon as often as he or she recommends, but no less than once per year to check the various parts of the new joint implant and make sure there are no other issues going no that need to be managed.
- Be mindful that your joint replacement is not the same as the original in terms of strength and resilience (especially to high impact activities), and the objective of your joint surgery was not to be come a triathlete, but live your life normally without debilitatiing pain all the time.
- Robert is again able to hike the rugged and beautiful Rocky Mountains around Denver, Colorado. By the end of 2008 Robert was almost unable to hike and an experience on a trail near Bailey, Colorado convinced him that he finally needed a knee replacement.
- For Francine Campone -- the lady who wrote the chapter on hip replacement -- the simple ability to go out and dance again and not be in misery.
- For you it might be bending over to play with a grand child, or going for a mall-crawl in the wintertime, however, while the above is a list of some personal reasons for going on the journey through joint replacement, there are other considerations for the rest of your life.